Limit risk through prevention
As the practice of aquaculture increases globally, more and more individuals will come into contact with zoonotic diseases specific to aquatic animals that have the potential to be transmitted to humans. Although there is an extensive list of pathogens that are infectious to humans via consumption of aquatic products, relatively few pathogens pose a risk to individuals who handle or come in contact with fish or their products.
No known viral or fungal pathogens are acquired by humans from fish solely through contact, and only a few reports of parasitic infections transmitted through the contact route have been recorded. Therefore, bacteria are the primary pathogens with zoonotic potential acquired through handling of fish (Table 1).
Smith, Potential zoonotic pathogens, Table 1
| Pathogen | Clinical Signs in Fish | Clinical Signs in Humans |
|---|---|---|
| Gram-negative Bacteria | ||
| Aeromonas species | Often non-specific, ulcerative skin lesions, abdominal distention, lethargy, exophthalmia, raised scales, fin erosion, death | Localized edema and swelling at site of infection, rarely systemic |
| Vibrio species | Often non-specific, lethargy, skin ulcers, abdominal distention, exophthalmia, fin erosion, death | Edema, tissue swelling, necrotizing fasciitis at site of infection |
| Gram-positive Bacteria | ||
| Mycobacterium species | Usually non-specific, lethargy, poor body condition, pigment changes, abdominal distention, scale loss, exophthalmia, skin ulcerations, death | Raised granulomatous nodules to ulcerative skin lesions, rarely systemic |
| Streptoccus iniae | Abdominal distention, hemorrhages of the skin, exophthalmia, death | Cellulitis, arthritis, endocarditis, meningitis, rarely death |
| Erysipelothrix rhusiopathiae | No apparent pathology | Localized to diffuse skin infection, endocarditis, death |
The majority of these pathogens are Gram-negative bacteria, but a few are Gram-positive bacteria associated with fish. Most are considered opportunistic in their infections of humans and are generally associated with trauma (cuts, abrasions, punctures) or immunocompromised individuals.
Gram-negative bacteria
Aeromonas species are ubiquitous in the freshwater aquatic environment and frequently cause disease in food, bait and ornamental fish. Non-specific clinical signs of Aeromonas infections in fish include ulcerative lesions of the skin, lesions around the bases of the fins and anus, raised scales, abdominal distension and exophthalmia. Aeromonad infections in fish are often secondary to stressors such as poor environmental conditions, including suboptimal temperatures and elevated ammonia or nitrite levels.
Aeromonas hydrophila, A. caviae, A. sobria and A. schubertii have all been implicated in human disease. The primary route of transmission is through contact with the mucus and tissues of infected fish. Existing cuts and abrasions on the hands, as well as puncture wounds from the fish are potential routes of infection. The most common sign of an Aeromonas infection in humans is localized swelling at the site of entry. However, in immunocompromised individuals, the infection can become systemic and prove life threatening.
Vibrio species are commonly isolated from marine and brackish water fish and environments due to the bacteria’s preference for higher salinities. In spite of this preference, a number of species of Vibrio can also be sporadically cultured from freshwater fish. These bacteria can cause disease in fish with non-specific clinical signs that include anorexia, lethargy, skin ulcers, exo-phthalmia and erythema around the anus and base of fins.
The most common Vibrio species in marine fish are V. vulnificus, V. parahemolyticus and V. cholera, with V. vulnificus the most common isolate in human infections. The major route of exposure in humans is through puncture wounds, with clinical signs of edema, tissue swelling and necrotizing fasciitis in the immediate area of the wound or abrasion.
There are occasional reports of other species of Gram-negative bacteria causing disease in humans from contact with fish. These bacteria in the genera Edwarsiella, Escherichia, Salmonella and Klebsiella are generally associated with freshwater fish or freshwater environments.
The most common routes of infection are through a puncture wound while handling or examining fish, or by infection of existing cuts and abrasions. Clinical signs of disease in fish can range from a localized infection of the skin to a more progressive systemic infection. An infection with any one of these bacteria in humans can be a localized inflammation at the point of entry or become systemic and result in severe illness.
Gram-positive bacteria
Infections with Mycobacterium species are probably the most common zoonotic infections acquired from fish. Numerous species of Mycobacterium have been cultured from fish, including M. marinum, M. fortuitum, M. chelonae, M. ulcerans, M. flavescens and M. gordonae. These aquatic bacteria belong to the non-tubercular group of mycobacterial pathogens and have been isolated from a wide range of freshwater, brackish water and marine species of fish. Any of these bacterial species can result in acute to chronic progressive disease in fish.
Generally few clinical signs are apparent with the acute form of the disease, and often only dead fish are found. Clinical signs associated with the chronic form of the disease include lethargy, poor body condition, pigment changes, abdominal distention, exophthalmia, scale loss and skin ulcers. Infected fish can serve as carriers of the disease without outward clinical signs of illness. The most likely route of transmission among fish is through the ingestion of infected feces or dead fish tissue. Sloughed tissue from infected gill or ulcerated skin lesions of live fish may also spread these organisms.
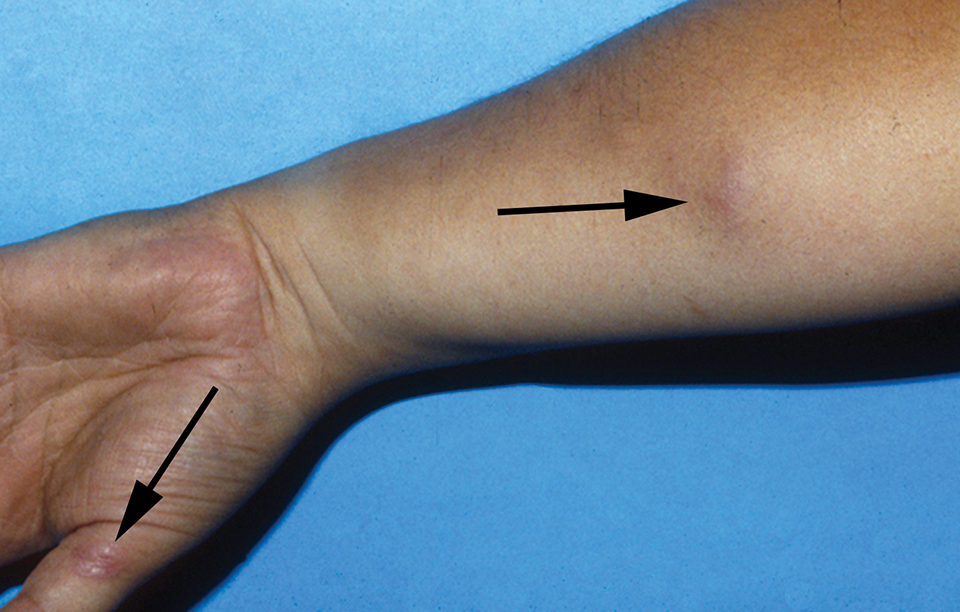
Zoonotic infections of Mycobacterium species in humans are often seen in individuals who handle or work with fish, leading to the common name “fish handlers disease” or “fish tank granuloma.” In humans, raised granulomatous nodules or ulcerative lesions generally occur on the hands and arms due to the bacteria’s preference for lower temperatures. Systemic mycobacteriosis has occurred in humans with resulting clinical signs of respiratory disease, but most of these cases were in immunocompromised individuals.
Streptococcus iniae causes abdominal distention, petechial hemorrhage of the dermis, exophthalmia and sometimes death in freshwater and marine species of fish. Many species of tropical and ornamental fish can harbor this bacterium, but several species of food fish appear predisposed to infection, including tilapia, striped bass and their hybrids.
Humans infected with S. iniae can exhibit clinical signs of cellulitis, systemic arthritis, endocarditis, meningitis and occasionally death. The major route of infection is through a puncture wound from the fish or infection of an existing wound.
Erysipelothrix rhusiopathiae is another bacterium that is ubi-quitous in freshwater and marine environments. Although no known pathology has been reported in fish, clinical signs of infection in humans can range from a localized to diffuse skin infection of the hands and fingers to a more progressive systemic infection in which the heart and heart valves are affected, resulting in endocarditis. As the bacterium is often associated with the mucus and skin of the fish, the typical route of infection is through contact or handling of contaminated fish tissues.
Prevention
Individuals who work with fish need to be aware of the zoonotic diseases that could be acquired from these aquatic animals. Obviously, the best way to prevent any chance of a zoonotic infection is to avoid contact with the fish and water. However, since this is generally not practical in aquaculture, then prevention is the best method for reducing the risk of acquiring these diseases.
Basic hygiene and thorough hand washing after contact with fish or water containing fish are the primary preventative measures for reducing this risk of exposure. Wearing gloves to protect open sores and cuts, reduce contact with the fish or water, and reduce potential injury from fish or equipment is another good way to prevent exposure to potential pathogens. Instead of hands, using brushes, scrubbers and sprayers for cleaning tanks, cages, netting and other equipment should also be encouraged.
Developing and implementing basic biosecurity procedures for an aquaculture facility are also important in reducing the introduction and spread of potential pathogens in an aquatic animal population. Such procedures can include establishing quarantine protocols for all new fish and eggs entering a facility to prevent contamination of established populations of fish and thereby reduce the potential exposure of humans to these pathogens.
New fish should be maintained in separate, isolated systems and held in quarantine for a minimum of 30 days while observing behavior, feeding responses and development of clinical signs or lesions. Regular health monitoring of fish in both the quarantined and existing populations is another way of insuring the identification of potential pathogens in a population. And finally, any individual working with fish who is seeking medical attention for lesions or illness of unknown origin should make their personal physician aware of their involvement with aquaculture.
(Editor’s Note: This article was originally published in the July/August 2011 print edition of the Global Aquaculture Advocate.)
Author
-
Stephen A. Smith, DVM, Ph.D.
Department of Biomedical Sciences and Pathobiology
Virginia-Maryland Regional College of Veterinary Medicine
Virginia Polytechnic Institute and State University
Blacksburg, Virginia 24061-0442 USA[117,100,101,46,116,118,64,55,104,116,105,109,115,116,115]
Tagged With
Related Posts
Intelligence
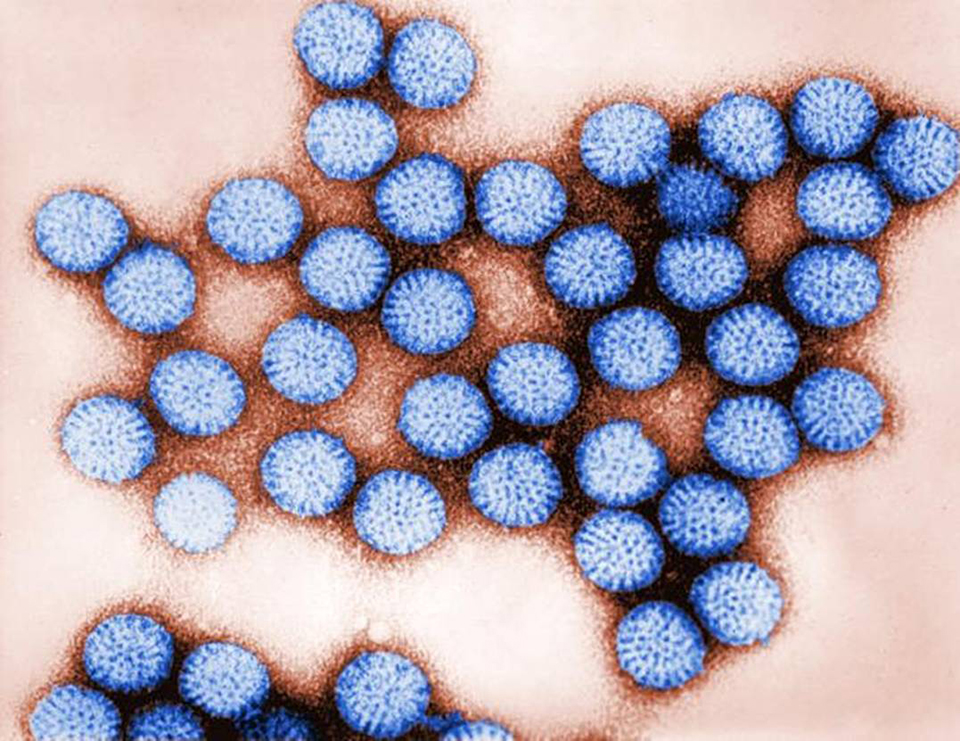
Human enteric viruses in shellfish, part 1
Commercially harvested shellfish have been reported to cause gastro-enteritis when humans consume virus-contaminated products. Rotaviruses are one of the main types of viruses able to survive and persist in the aquatic environment.

Intelligence
As ocean temperatures rise, so too will vibrio outbreaks
A study using a half-century of data has linked climate change and warming sea temperatures with an increase in illnesses from the common vibrio bacteria. Shellfish growers, fighting a particularly virulent strain of Vibrio parahaemolyticus, are changing their harvest protocols.

Health & Welfare
Biosecurity: Not just a word
Most aquaculture farms rely on general strategies for biosecurity that implement protocols learned from others. Establishing effective biosecurity, however, can be complicated due to multiple interacting variables.

Health & Welfare
Temperature affects quality, safety of quahog clams
The rapid cooling of harvested quahog clams to achieve the product temperatures required by regulators and dealers can often result in mortalities due to thermal shock.


